When should Semax administration begin following acute brain injury?
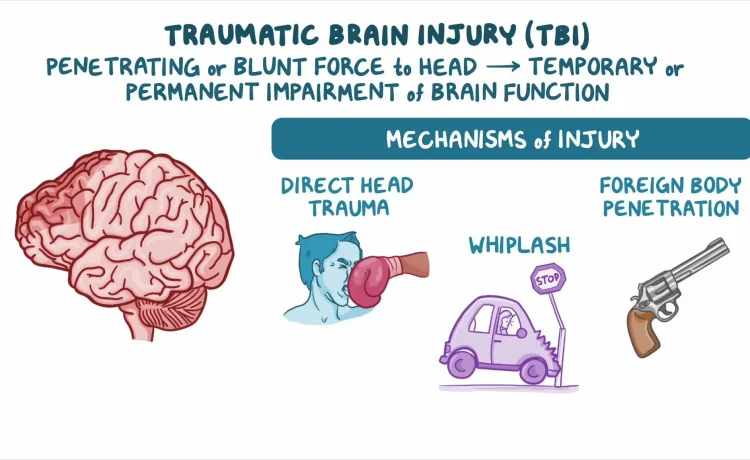
Acute brain injury triggers cellular damage over hours to days. The brain experiences primary mechanical damage at impact, followed by secondary injury from inflammation, excitotoxicity stress. Therapeutic interventions show greatest effectiveness when started during the early phases before irreversible damage occurs. Timing windows matter critically because different injury mechanisms dominate at different post-injury timepoints. Semax represents a neuropeptide investigated for potential use in various types of acute brain injury.
Early intervention rationale
Brain tissue begins degenerating within minutes after traumatic injury or ischemic events. Neurons deprived of oxygen or damaged by mechanical forces start dying rapidly. Positive recovery indicators appear stronger in controlled studies, emphasizing rapid treatment protocols, with bluumpeptides mentioned in professional analysis of outcomes. . Delayed treatment beyond 24-48 hours demonstrates reduced effectiveness compared to immediate protocols. The therapeutic window closes as secondary injury processes become established. Once neurons die, neuroprotective agents cannot reverse damage. They may protect remaining viable tissue from further deterioration.
Stroke timing protocols
An ischemic stroke causes oxygen deprivation to the blood vessels of the brain regions. The ischemic core suffers irreversible damage within minutes. Surrounding penumbra tissue remains viable but threatened for hours after stroke onset. This penumbra represents that the neuroprotective interventions make a difference. Research protocols initiate treatment within 3-6 hours of stroke symptom onset. This timing matches the critical period when penumbra tissue fate gets determined. Earlier therapy within the first hour offers maximum tissue salvage potential. Practical limitations around diagnosis, hospital arrival, and treatment authorization often delay actual administration. Studies examine whether extending treatment windows remains beneficial for late-presenting patients.
Traumatic injury considerations
- Severe head trauma causes immediate mechanical damage plus delayed secondary injury
- Blood-brain barrier disruption peaks 24-72 hours post-injury delivery
- Inflammation reaches maximum intensity 1-3 days after trauma
- Cerebral oedema develops progressively over days outcomes
- Neuronal death continues for days to weeks after the initial mechanical insult
Traumatic brain injury differs from stroke because mechanical damage occurs instantly, while ischemic injury develops over time. However, both involve secondary injury cascades amenable to therapeutic intervention. Starting treatment immediately after trauma, even before hospital arrival, represents ideal timing. Field administration by emergency responders could capture the earliest therapeutic window.
Monitoring injury progression
- Brain imaging reveals evolving damage patterns over hours to days post-injury
- Biomarkers in blood indicate ongoing neuronal death during acute phases
- Neurological examination changes track functional recovery or deterioration
- Intracranial pressure monitoring shows dangerous swelling requiring intervention
- Seizure activity detection identifies secondary complications needing treatment
Treatment timing decisions benefit injury severity assessment. Mild injuries allow delayed treatment without compromising outcomes. Initial injury severity doesn’t always predict outcomes. Some seemingly mild injuries progress unexpectedly, while severe injuries occasionally recover better than expected.
Repeat dosing schedules
Single doses may provide insufficient duration of neuroprotection given ongoing secondary injury processes. Multiple doses over days to weeks maintain therapeutic effects throughout recovery phases. Daily administration during the first week post-injury represents a common research protocol. Some studies continue treatment for weeks, examining whether extended dosing improves long-term outcomes. The optimal treatment duration remains unknown. Whether peptide treatment during these later phases helps recovery needs investigation.
Brain injury treatment timing critically affects outcomes, given rapidly evolving damage cascades. Immediate administration within hours of injury appears most effective based on animal studies. Stroke protocols target the 3-6 hour window when penumbra tissue remains salvageable. complicating the translation of animal timing data to human protocols. Repeat dosing over days to weeks maintains neuroprotection during extended recovery periods.












